Endovascular management of the rectus muscle hematoma
Stefano Pieri, Paolo Agresti, Grazia Loretta Buquicchio, Ilenia Di Giampietro, Margherita Trinci, Vittorio Miele
Abstract
Purpose Non-traumatic spontaneous hematoma of the rectus abdominal muscle is not considered a critical condition. Nevertheless, it can be a serious complication in some patients due to continuous and/or consistent bleeding. The most frequent cause of spontaneous rectus muscle hematoma is the anticoagulation therapy. The natural history of rectus muscle hematoma usually leads to a positive outcome and can be spontaneously self-limited only by conservative therapy. Nevertheless, in some patients, despite a correct and early medical therapy, the continuous bleeding requests a more radical handling. Up to now, the surgical hematoma evacuation and the bonding of blood vessels were considered the most appropriate treatment, while at present, the percutaneous management by means of selective catheters and embolization of the bleeding vessel is considered to be the most used option. Our purpose is to report our experience in the endovascular spontaneous rectus muscle bleeding treatment in the elderly patients.
Materials and methods From the data base and medical reports of the hospital, we selected 144 medical reports.
We focused on those cases that showed the following criteria: patients with rectus muscle hematoma undergoing anticoagulation therapy and/or non-traumatic spontaneous hematoma and with persistent bleeding revealed on CT examination despite a pharmacological treatment aimed to timely reverse coagulopathy. These criteria were found in 18 patients: 15 females and 3 males, with a median age of 73 (range 64–81). In all patients, the diagnosis had been confirmed by an abdominal CT in emergency setting, performed before and after contrast medium intravenous administration. Because of clinical conditions, all patients had been moved on the angiographic room for diagnostic arteriography and embolization. The criteria for this treatment were hemodynamic instability and the continuous bleeding despite the correct medical therapy.
Results CT imaging detected rectus muscle hematoma in 18/18 patients and active bleeding in 7/18 patients. Selective catheterization was applied to all 18 patients; arteriographic study confirmed the information of the CT study in all of the seven patients. The inferior epigastric artery was the main cause of the bleeding in all 18 patients. In 14 patients, one single vessel was responsible for the bleeding, while in the other four patients, more than one vessel were involved: In two patients, we also found the involvement of the superior epigastric artery; while the other two patients showed also the involvement of the deep iliac circumflex artery. The material for embolization was compatible coils with microcatheters in 17/18 patients, and glue for 1/18 patient.
Conclusions Patients with large rectus muscle hematoma, which have not yet recovered with conservative therapy, should then consider undergoing endovascular treatment. This procedure is highly recommended in patients with other coexisting pathologies that could eventually lead to a fatal outcome. It is difficult to determine when surgery is necessary when there is very poor data provided by scientific literature review, so the decision to use surgery can be suggested when embolization is unsuccessful or when it is necessary to evacuate a complex huge fluid mass in peritoneal cavity.
Introduction
The rectus muscle hematoma is a blood collection in the sheath of the anterior rectus muscle, due to epigastric artery damage or the tearing of one or more muscle fibers, usually located beneath the umbilicus where blood vessels are not protected by external aponeurotic fascia [1]. Non-traumatic spontaneous hematoma of the rectus abdominal muscle is not a common cause of pain in ordinary medical treatment, and it is not considered a critical condition [2, 3]. Nevertheless, it can be a serious complication in some patients due to continuous and/or consistent bleeding [4].
The most frequent cause of spontaneous rectus muscle hematoma is the anticoagulation therapy [5, 6]. The natural history of rectus muscle hematoma usually leads to a positive outcome and can be spontaneously self-limited only by conservative therapy [7]. Nevertheless, a large hematoma can develop and/or cause a severe hypovolemia that requests not only an early and accurate medical instrumental diagnosis and treatment, but also an adequate therapy with an inversion of the coagulation cascade, liquid infusion and hemostatic treatment [8].
In some patients, despite a correct and early medical therapy, the continuous bleeding requests a more radical handling [8, 9]. Up to now, the surgical hematoma evacuation and the bonding of blood vessels were considered the most appropriate treatment, while at present, the percutaneous management by means of selective catheters and embolization of the bleeding vessel is considered to be the most used option [10].
Our purpose is to report our experience in the endovascular spontaneous rectus muscle bleeding treatment in the elderly patients.
Materials and methods
Going through the data base and medical reports of the hospital, we focused on those medical cases that emphasized “rectus muscle hematoma” in the main diagnosis, which occurred between the year 2001 through 2011. From the selected 144 medical reports, we focused on those cases that showed the following criteria: patients with rectus muscle hematoma undergoing anticoagulation therapy and/or non-traumatic spontaneous hematoma and with persistent bleeding revealed on CT examination despite a pharmacological treatment aimed to timely reverse coagulopathy.
These criteria were found in 18 patients: 15 females and 3 males, with a median age of 73 (range 64–81 years). 10/18 patients had acute and oppressive pain status in the lower abdomen and abdominal swelling which ultrasound had confirmed to be pertaining to the superficial tissue (Fig. 1a, b).
The symptoms had become acute after a cough in nine cases, after Valsalva maneuver in four cases, after a chest torsion in three cases and for unknown causes in two cases. Upon arrival at the hospital, all patients had low hemoglobin levels, at least −4 points percentage which had a further drop despite the medical therapy in 5/8 patients, causing a hypovolemic shock; the other patients showed a stable hemodynamic condition.
In all patients, the diagnosis was confirmed by an abdominal CT (Light Speed 16 General Electric), in emergency setting (Fig. 2a–c), performed before and after contrast medium intravenous administration. CE-MDCT protocol includes arterial and venous phase scans. A nonionic contrast medium volume of 120–150 ml was injected, at 3–4 ml/s through a 18–20 G needle. Arterial active bleeding was diagnosed when CT scans demonstrated within the hematoma a focal or diffuse area of high attenuation that was isodense with adjacent arterial vessels. A delay ranging from 30 to 40 s was used for the arterial phase and from 70 to 80 s for the venous phase.
Because of clinical conditions, all patients were moved on the angiographic room for diagnostic arteriography and embolization (OEC 9800 Plus-General Electric). The criteria for this treatment were hemodynamic instability (arterial pressure below 90/60 mmHg despite therapy) and the continuous bleeding despite the correct medical therapy (so the patient continued to have symptoms or the hematoma continued to grow) [13–18].
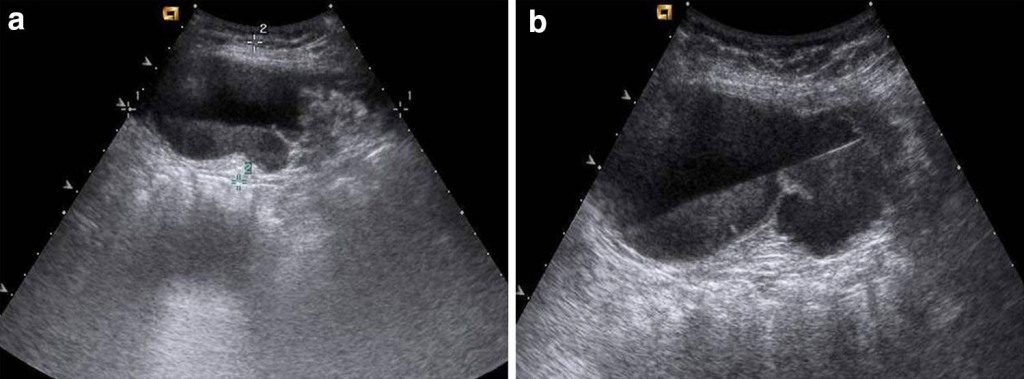 Fig. 1 Ultrasound: diagnos tic study, carried out with a 15-MHz linear probe, detects a subcutaneous fluid collection, with a superior hypoechoic portion and a slightly hyperechoic inferior part: The patient’s position determines the obliquity of the blood level gathered in the fluid collection
Fig. 1 Ultrasound: diagnos tic study, carried out with a 15-MHz linear probe, detects a subcutaneous fluid collection, with a superior hypoechoic portion and a slightly hyperechoic inferior part: The patient’s position determines the obliquity of the blood level gathered in the fluid collection
 Fig. 2 CT: triphasic CT examination (basal phase, arterial phase and venous phase) allows to determine the topographic, morphological and functional characteristics of the hematoma. The CT basal phase a reveals a mass effect developing toward the abdominal cavity in the same level shown in US examination, with a slightly low hyperdensity, as if a recent bleeding had occurred. The CT arterial phase b shows an active bleeding in the hematoma: Irregular aspects of the arterial vessel confirm the presence of injury causing the bleeding outcome. Lower level scans c allows to follow the bleeding arterial branch, the lower epigastric artery in this specific case, providing important data to request interventional radiology for further management
Fig. 2 CT: triphasic CT examination (basal phase, arterial phase and venous phase) allows to determine the topographic, morphological and functional characteristics of the hematoma. The CT basal phase a reveals a mass effect developing toward the abdominal cavity in the same level shown in US examination, with a slightly low hyperdensity, as if a recent bleeding had occurred. The CT arterial phase b shows an active bleeding in the hematoma: Irregular aspects of the arterial vessel confirm the presence of injury causing the bleeding outcome. Lower level scans c allows to follow the bleeding arterial branch, the lower epigastric artery in this specific case, providing important data to request interventional radiology for further management
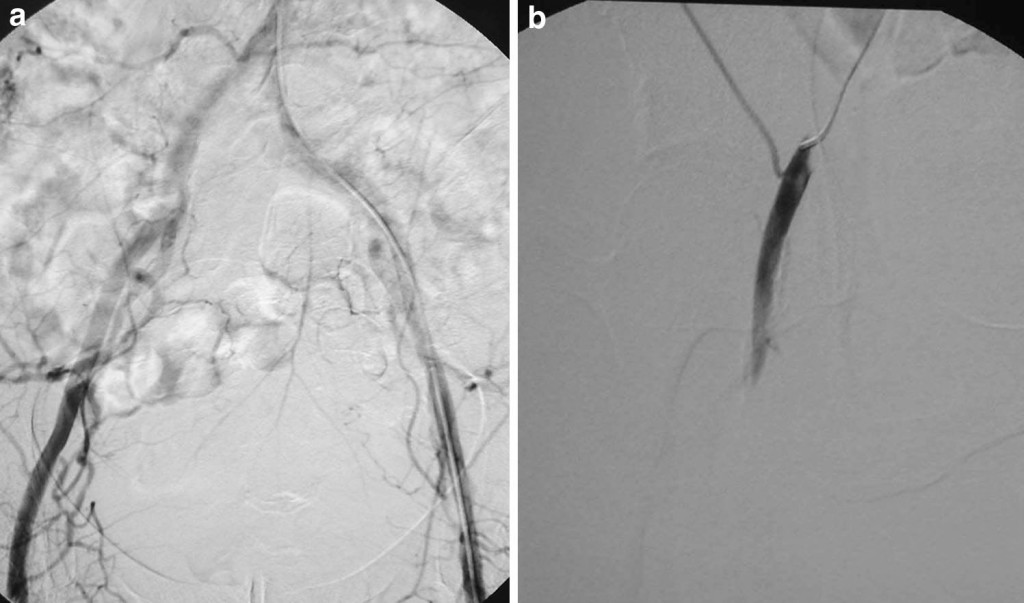 Fig. 3 Angiography: arteriographic examination is performed by opposite side transfemoral access as to the hematoma and consists in an aortoiliac panoramic study, to have an overall anatomic visual reference (a); at this point, through selective catheterism, it is possible to point out the origin of the lower epigastric artery (b), providing an essential anatomic map for the following super-selective catheterism by micro-catheters
Fig. 3 Angiography: arteriographic examination is performed by opposite side transfemoral access as to the hematoma and consists in an aortoiliac panoramic study, to have an overall anatomic visual reference (a); at this point, through selective catheterism, it is possible to point out the origin of the lower epigastric artery (b), providing an essential anatomic map for the following super-selective catheterism by micro-catheters
The transfemoral diagnostic arteriography was carried out after local anesthesia, on the opposite side of the hematoma (Fig. 3a); the vascular access was performed by means of a vascular sheath of 5 Fr (Terumo Europe, Leuven, Belgium). After the overall study of the abdominal aorta and of the iliac vessels, a selective catheterization of the external iliac artery was performed, highlighting the anatomic characteristics of the vessels originating (Fig. 3b).
The choice of the angiographic catheter (cobra, headhunter, multipurpose, Cordis Europe) was made considering the morphology of the specific vessel.
The study of the damaged artery and its interventistic treatment were carried out by means of a micro-catheter 3 Fr, coaxial as respect to the angiographic one (Progreat 2,8 Fr-Terumo Europe, Leuven, Belgium); coils (Tornado–Cook Europe, Denmark) and/or other embolization material (Curaspon, Curamedical, BV, NetherlandsGlubran 2, GEM srl, Viareggio, Italy) was used to stop the bleeding: The choice was based on the characteristics of the wound (anatomic location and size of the bleeding vessel).
The absence of contrast material extravasation during a further arteriography, performed at the end of the treatment, was considered to be the crucial criteria determining the technical success of the overall operation.
The increase in the hemodynamic and hemoglobin values was considered a medical success.
Results
Preliminary CT studies were performed in all 18 patients and detected hematomas in 18/18 patients.
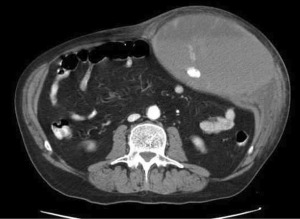 Fig. 4 CT: large left-sided rectus muscle hematoma extending its mass effect to the homolateral flank; it is possible to depict a wellshaped mass rim, a mass effect toward the inside, a fluid level with hyperdensity of the declive portion due to recent bleeding and the presence of an active bleeding. The contrast material pooling shows the same density as that in aorta
Fig. 4 CT: large left-sided rectus muscle hematoma extending its mass effect to the homolateral flank; it is possible to depict a wellshaped mass rim, a mass effect toward the inside, a fluid level with hyperdensity of the declive portion due to recent bleeding and the presence of an active bleeding. The contrast material pooling shows the same density as that in aorta
In 11/18 patients, CT scans demonstrated only the presence of hematoma, with no active bleeding. In 7/18 patients, CT showed an active bleeding within the hematoma (Fig. 4). In this seven cases, active bleeding was considered to be in the territory of the inferior epigastric artery in 5/7 cases and in the territory of the superior epigastric artery in 2/7 cases (Fig. 5).
Selective catheterization was applied to all patients; arteriographic study confirmed the site of the bleeding in all of the seven patients in whose CT demonstrated it.
The inferior epigastric artery was the main cause of the bleeding in all 18 patients. In 14/18 patients, one single vessel was responsible for the bleeding, while in the other 4/18 patients, more than one vessel were involved: In two patients, we also found the involvement of the superior epigastric artery, while the other two patients showed also the involvement of the deep iliac circumflex artery.
The embolization material used was compatible coils with micro-catheters in 17/18 patients, and glue for one patient. Embolization was carried out with success, since no active bleeding was revealed during arteriography at the end of the endovascular treatment.
15/18 patients were submitted to an 18-day CT followup. During this period, no further or new bleeding was revealed, and hemodynamic levels were stabilized: Blood pressure had become normal in 14/18 patients; only four patients were treated with blood transfusion to correct anemia, and only one patient needed platelet therapy. None of the cases requested surgery.
Contrast-enhanced ultrasound (CEUS) carried out only in 7/18 patients proved no active bleeding. No further complication was reported neither during nor after embolization procedures; 3/18 patients died during hospitalization (the first after 12 h, the second after 2 days and the last after 8 days), due to multiorgans failure as a result of hemodynamic disorders due to the hematoma: severe kidney failure in two cases and heart failure in one case.
Conclusions
Patients with large rectus muscle hematoma, which have not yet recovered with conservative therapy, should then consider undergoing endovascular treatment.
This procedure is highly recommended in patients with other coexisting pathologies that could eventually lead to a fatal outcome.
It is difficult to determine when surgery is necessary when there is very poor data provided by scientific literature review, so the decision to use surgery can be suggested when embolization is unsuccessful or when it is necessary to evacuate a complex huge fluid mass in peritoneal cavity.
Puoi leggere i dettagli e i riferimenti bibliografici scaricando il documento completo: Endovascular management of the rectus muscle hematoma.
Per altre informazioni sull’ematoma del muscolo retto puoi visitare la pagina nella sezione patologie: ematoma del muscolo retto.